Seasonal Affective Disorder Vitamin D
Seasonal Affective Disorder
- Download PDF
- Download ePub
- Order a free hardcopy
- En español
What is seasonal affective disorder?
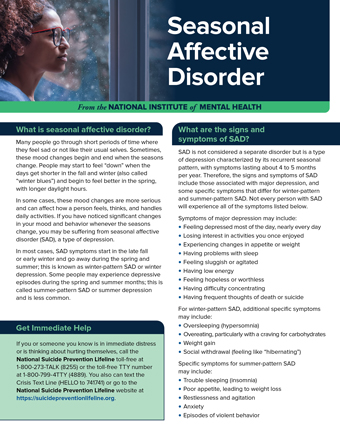
Many people go through short periods of time where they feel sad or not like their usual selves. Sometimes, these mood changes begin and end when the seasons change. People may start to feel "down" when the days get shorter in the fall and winter (also called "winter blues") and begin to feel better in the spring, with longer daylight hours.
In some cases, these mood changes are more serious and can affect how a person feels, thinks, and handles daily activities. If you have noticed significant changes in your mood and behavior whenever the seasons change, you may be suffering from seasonal affective disorder (SAD), a type of depression.
In most cases, SAD symptoms start in the late fall or early winter and go away during the spring and summer; this is known as winter-pattern SAD or winter depression. Some people may experience depressive episodes during the spring and summer months; this is called summer-pattern SAD or summer depression and is less common.
What are the signs and symptoms of SAD?
SAD is not considered a separate disorder but is a type of depression characterized by its recurrent seasonal pattern, with symptoms lasting about 4 to 5 months per year. Therefore, the signs and symptoms of SAD include those associated with major depression, and some specific symptoms that differ for winter-pattern and summer-pattern SAD. Not every person with SAD will experience all of the symptoms listed below.
Symptoms of major depression may include:
- Feeling depressed most of the day, nearly every day
- Losing interest in activities you once enjoyed
- Experiencing changes in appetite or weight
- Having problems with sleep
- Feeling sluggish or agitated
- Having low energy
- Feeling hopeless or worthless
- Having difficulty concentrating
- Having frequent thoughts of death or suicide
For winter-pattern SAD, additional specific symptoms may include:
- Oversleeping (hypersomnia)
- Overeating, particularly with a craving for carbohydrates
- Weight gain
- Social withdrawal (feeling like "hibernating")
Specific symptoms for summer-pattern SAD may include:
- Trouble sleeping (insomnia)
- Poor appetite, leading to weight loss
- Restlessness and agitation
- Anxiety
- Episodes of violent behavior
Get Immediate Help
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
How is SAD diagnosed?
If you think you may be suffering from SAD, talk to your health care provider or a mental health specialist about your concerns. They may have you fill out specific questionnaires to determine if your symptoms meet the criteria for SAD.
To be diagnosed with SAD, a person must meet the following criteria:
- They must have symptoms of major depression or the more specific symptoms listed above.
- The depressive episodes must occur during specific seasons (i.e., only during the winter months or the summer months) for at least 2 consecutive years. However, not all people with SAD do experience symptoms every year.
- The episodes must be much more frequent than other depressive episodes that the person may have had at other times of the year during their lifetime.
Who develops SAD?
Millions of American adults may suffer from SAD, although many may not know they have the condition. SAD occurs much more often in women than in men, and it is more common in those living farther north, where there are shorter daylight hours in the winter. For example, people living in Alaska or New England may be more likely to develop SAD than people living in Florida. In most cases, SAD begins in young adulthood.
SAD is more common in people with major depressive disorder or bipolar disorder, especially bipolar II disorder, which is associated with recurrent depressive and hypomanic episodes (less severe than the full-blown manic episodes typical of bipolar I disorder). Additionally, people with SAD tend to have other mental disorders, such as attention-deficit/hyperactivity disorder, an eating disorder, an anxiety disorder, or panic disorder. Learn more about these disorders by visiting the NIMH Mental Health Information page.
SAD sometimes runs in families. SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.
What causes SAD?
Scientists do not fully understand what causes SAD. Research indicates that people with SAD may have reduced activity of the brain chemical (neurotransmitter) serotonin, which helps regulate mood. Research also suggests that sunlight controls the levels of molecules that help maintain normal serotonin levels, but in people with SAD, this regulation does not function properly, resulting in decreased serotonin levels in the winter.
Other findings suggest that people with SAD produce too much melatonin—a hormone that is central for maintaining the normal sleep-wake cycle. Overproduction of melatonin can increase sleepiness.
Both serotonin and melatonin help maintain the body's daily rhythm that is tied to the seasonal night-day cycle. In people with SAD, the changes in serotonin and melatonin levels disrupt the normal daily rhythms. As a result, they can no longer adjust to the seasonal changes in day length, leading to sleep, mood, and behavior changes.
Deficits in vitamin D may exacerbate these problems because vitamin D is believed to promote serotonin activity. In addition to vitamin D consumed with diet, the body produces vitamin D when exposed to sunlight on the skin. With less daylight in the winter, people with SAD may have lower vitamin D levels, which may further hinder serotonin activity.
Negative thoughts and feelings about the winter and its associated limitations and stresses are common among people with SAD (as well as others). It is unclear whether these are "causes" or "effects" of the mood disorder, but they can be a useful focus of treatment.
How is SAD treated?
Treatments are available that can help many people with SAD. They fall into four main categories that may be used alone or in combination:
- Light therapy
- Psychotherapy
- Antidepressant medications
- Vitamin D
Talk to your health care provider about which treatment, or combination of treatments, is best for you. For tips for talking with your health care provider, refer to the NIMH fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Light Therapy
Since the 1980s, light therapy has been a mainstay for the treatment of SAD. It aims to expose people with SAD to a bright light every day to make up for the diminished natural sunshine in the darker months.
For this treatment, the person sits in front of a very bright light box (10,000 lux) every day for about 30 to 45 minutes, usually first thing in the morning, from fall to spring. The light boxes, which are about 20 times brighter than ordinary indoor light, filter out the potentially damaging UV light, making this a safe treatment for most. However, people with certain eye diseases or people taking certain medications that increase sensitivity to sunlight may need to use alternative treatments or use light therapy under medical supervision.
Psychotherapy or "Talk Therapy"
Cognitive behavioral therapy (CBT) is a type of talk therapy aimed at helping people learn how to cope with difficult situations; CBT also has been adapted for people with SAD (CBT-SAD). It is typically conducted in two weekly group sessions for 6 weeks and focuses on replacing negative thoughts related to the winter season (e.g., about the darkness of winter) with more positive thoughts. CBT-SAD also uses a process called behavioral activation, which helps individuals identify and schedule pleasant, engaging indoor or outdoor activities to combat the loss of interest they typically experience in the winter.
When researchers directly compared CBT with light therapy, both treatments were equally effective in improving SAD symptoms. Some symptoms seemed to get better a little faster with light therapy than with CBT. However, a long-term study that followed SAD patients for two winters found that the positive effects of CBT seemed to last longer over time.
Medications
Because SAD, like other types of depression, is associated with disturbances in serotonin activity, antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are also used to treat SAD when symptoms occur. These agents can significantly enhance patients' moods. Commonly used SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
The U.S. Food and Drug Administration (FDA) also has approved another type of antidepressant, bupropion, in an extended-release form, that can prevent recurrence of seasonal major depressive episodes when taken daily from the fall until the following early spring.
All medications can have side effects. Talk to your doctor about the possible risk of using these medications for your condition. You may need to try several different antidepressant medications before finding one that improves your symptoms without causing problematic side effects. For basic information about SSRIs, bupropion, and other mental health medications, visit the NIMH Mental Health Medications page. Also, visit the FDA website for the most up-to-date information on medications, side effects, and warnings.
Vitamin D
Because many people with SAD often have vitamin D deficiency, nutritional supplements of vitamin D may help improve their symptoms. However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
Can SAD be prevented?
Because the timing of the onset of winter pattern-SAD is so predictable, people with a history of SAD might benefit from starting the treatments mentioned above before the fall to help prevent or reduce the depression. To date, very few studies have investigated this question, and existing studies have found no convincing evidence that starting light therapy or psychotherapy ahead of time could prevent the onset of depression. Only preventive treatment with the antidepressant bupropion prevented SAD in study participants, but it also had a higher risk of side effects. Therefore, people with SAD should discuss with their health care providers if they want to initiate treatment early to prevent depressive episodes.
Are there clinical trials studying SAD?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions—including SAD. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information about clinical research and how to find clinical trials being conducted around the country, visit the NIMH Clinical Trials page.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, refer to our reprint guidelines.
For More Information
MedlinePlus (En español)
ClinicalTrials.gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-8138
Seasonal Affective Disorder Vitamin D
Source: https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder








Tidak ada komentar:
Posting Komentar